Outpatient consultations
Secretaries
- Opening hours: Monday to Friday, 9am to 5pm
- Telephone: +33(0)2 31 45 50 40
- Location: 1st floor
- Secure e-mail for external healthcare professionals: cfb.cmca.baclesse@medical14.apicrypt.org
- Secure e-mail for hospital healthcare professionals: cfb.cmca.baclesse@medical14.apicrypt.fr
Hospitalisation
Intermediate Care Unit
- Visiting hours: Monday to Sunday, 2pm to 8pm
- Nursing office: Call the switchboard at +33(0)2 31 45 50 50 and ask for the USC (IMC) nurses’ office.
- Location: 1st floor
- Secure e-mail for external healthcare professionals: cfb.cmca.baclesse@medical14.apicrypt.org
- Secure e-mail for hospital healthcare professionals: cfb.cmca.baclesse@medical14.apicrypt.fr
Department missions
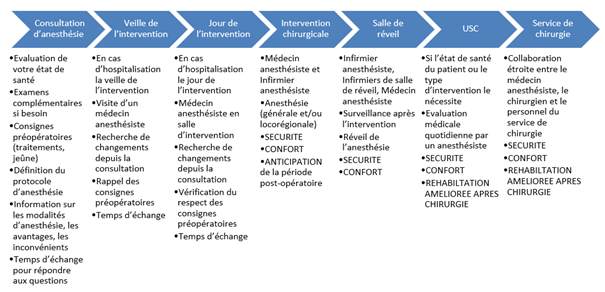
The key mission of the anaesthesiology team is to ensure safety and comfort for patients throughout their peri-operative care, from the anaesthesiology consultation to hospital discharge after surgery.
The anaesthesiology team ensures a number of transversal missions:
- Care: installation of venous access devices, vital emergency care throughout the centre.
- In close collaboration with other departments and participation in commissions: CUV (vital emergency commission), pain management team and CLUD (pain management committee), nutrition team and food and nutrition liaison committee (CLAN), haemovigilance and CSTH (transfusion safety and haemovigilance committee), quality department, pharmacy and COMEDIMS (medical and sterile medical devices committee) etc…
- Teaching: AFGSU (training certificate in emergency procedures and care) training, medical intern training, emergency situation in the operating theatre training, etc.
- University training: an anaesthesiology intern is a member of the team and intervenes in the operating theatre, in consultations and in the intermediate care unit, under constant supervision by the senior anaesthesiology physician.
- Research: research projects within the framework of theses and dissertations, participation in research work with other establishments, etc.
The department’s professionals
Head of department:
- Dr Vincent Leprince
Nursing supervisor: Eric Anger
Anaesthesiologists:
- Dr Edouard Caspersen
- Dr Axel Coquerel
- Dr Christine Dessaux
- Dr Marine Hubert
- Dr Vincent Leprince
- Dr Eléonore Mulac-Vauclair
- Dr Pierre Verrier
- Dr Alexandre Uk Hel Chau
Other professionals: > 1 medical assistant: Corinne Marie
For the operating theatre: > 12 state-qualified nurse anaesthetists > 1 state-qualified nurse for the recovery room
For the surgery departments and the Intermediate Care Unit: > 15 state-qualified nurses > 9 nursing auxiliaries
Care offer, expertise and specific training
Our care actvities
Expertise
- General anaesthesiology: a highly versatile anaesthesiology team, techniques adapted to each surgical procedure, the patient’s health status and the specificities of cancer care (Opoid Free anaesthesia technique, command of difficult intubation techniques). Particular expertise in peri-operative management of major referral surgery that is not available in other establishments (e.g. HIPEC, complex sarcoma exeresis, etc.)
- Locoregional anaesthesiology: alone or associated with general anaesthesiology, enables improved pain management and post-surgical recovery (spinal anasthaesia for digestive and gynaecological surgery, specific locoregional anaesthesia techniques for breast cancer, etc.)
- Hypnosis: Medical hypnosis is part of a dynamic strategy to improve the quality of patient care in the operating theatre and in the surgical department. Several medical and paramedical professionals are trained or currently undergoing training in hypnosis. Awareness of all theatre staff has been increased thanks to a video on positive communication.
- Implantation of central venous access devices (PICC lines in particular) under local anaethesia upon request by other centre physicians, to enable certain specific treatment to be administered.
- IMC (Intermediate Care Unit) and emergency management: mangement of peri-operative nutrition in association with the mobile nutrition team, of post-operative pain and of post-operative complications.
- Enhanced recovery after surgery (ERAS): the anaesthesiology team actively participates in the ERAS programme, enabling faster recovery after surgery.
- Patient blood management: to optimise peri-operative care, particular attention is paid to anaemia management by the anaesthesiology team (decrease in haemoglobin levels = lack of red blood cells). Adapted care is administered on a case-by-case basis depending on the type of surgery and on each patient’s health status
- Green Surgery: sustainable development approach in the operating theatre spurred by nurse anaesthetists and followed by all theatre staff.
Specific training
All resuscitation anaesthesiologists in the team are versatile and work equally in the operating theatre, in consultation, and in the intermediate care unit. They strive to remain trained in the latest techniques throughout their career in order to offer patients the best possible care, in line with the latest medical advances.
- Locoregional anaesthesiology and pain management: Dr Mulac-Vauclair and Dr Lafosse both hold a post-graduate diploma in locoregional anaesthesia. Dr Leprince holds a post-graduate diploma in pain management.
- Hypnosis: Dr Butin is currently undergoing training (year 2020) in medical hypnosis. Dr Dessaux has been practicing hypnosis for several years. Stéphanie Gibier is a state-qualified nurse anaesthetist trained in hypnosis.
- Cardiac ultrasound: Dr Leprince holds a post-graduate diploma in ultrasound techniques in anaesthesiology-reanimation (cardiac ultrasound option) and Dr Verrier holds a post-graduate diploma in cardiac ultrasound.
- Reanimation: Dr Coquerel holds a post-graduate diploma in reanimation in infectious diseases and a post-graduate oncology diploma in medical reanimation. Dr Verrier holds a post-graduate oncology diploma in medical reanimation and a post-graduate diploma in nephrology reanimation.
- Medical simulation: Dr Butin and Michèle Marie, state-qualified nurse anaesthetist, are trainers in medical simulation.
- Practical training in paediatric anaesthesiology for the entire team.
- Adapted physical education: Dr Coquerel is currently undergoing training (year 2020) towards a sports medicine capacitation.
The department’s equipment and facilities
- IMC (Intermediate Care Unit): monitors, ventilators, defibrillator
- Operating room, post-operative recovery room and interventional radiology or brachytherapy rooms: monitors, ventilators, defibrillators, ultrasound machines, virtual reality headset, anaesthesia and analgesia monitors, NMBA monitors, fluid warming systems and heated blankets, oesophageal Doppler, Pulsioflex haemodynamic monitor.
Department results
2019 activity data
- 3,409 procedures under general anaesthesia
- 3,365 aneasthesiology consultations
- 407 PICC line implantations
- 403 hospitalisations in the IMC
Research themes / Projects
- E-consult: interactive visual aid for providing patients with information on aneasthesia during consultation.
- Development of teleconsultation: possibility for (certain) patients to benefit from remote anaesthesiology consultations, depending on the type of procedure.
- Thoracic epidural: implementation of this locoregional anaesthesia technique, which is beneficial for certain procedures.
- Integration of adapted physical education in the ERAS (enhanced recovery after surgery) programme
Partnerships
At regional level: CHU university hospital in Caen for the hosting of medical interns and student nurses and participation in research projects
At national level: Institut Curie for practical training in paediatric anasthaesiology in proton therapy
Dispensed training
- Initial training: AFGSU
- Conintuing education: AFGSU ‘refresher’
- Lectures at the nursing school for aneasthesiology nurses
- Training and simulation for IMC staff: vasopressors, cardio-respiratory arrest, rapid sequence induction.

